
What’s your favorite burger? Is it in the picture above? (Sorry if you are reading this while hungry). How can burgers help us to understand Autism Spectrum disorder? Burgers have different toppings; some have cheese, some have eggs, some have lettuce, and some have tomatoes, while some are purely Vegan. However, One striking similarity is that, whatever the toppings, they all have buns. The buns may vary; we can have Potato Burger Buns, Brioche Burger Buns, or even Black Brioche Buns.
In the same way, Autism Spectrum Disorder has its “buns.” These are the common signs that all children with this Developmental disorder have.
The “buns” (common) signs of Autism Spectrum Disorder is:
- Impairment in Social interaction and verbal communication, and
- A narrow range of interests, routines and repetitive behaviors.
Other signs may be present in some children with Autism Spectrum Disorder and not show in others. These are the “topping” signs. They include:
- A reduction in imagination, ideas, and creativity.
- Limited gestures and non-verbal communication.
- Unusual sensory responses (Sensory Processing Disorder or Sensory Integration Difficulties)
This article looks at one of the “topping” signs of Autism Spectrum Disorder – Sensory Processing Disorder. Often, children with Autism Spectrum Disorder (A.S.D.) will have Sensory Processing Disorder (S.P.D.). However, not all children with Sensory Processing Disorder are Autistic (that’s why we called it a “topping” sign). A child can have Sensory Processing Disorder, a condition not linked to Autism Spectrum Disorder.
What is Sensory Processing Disorder?
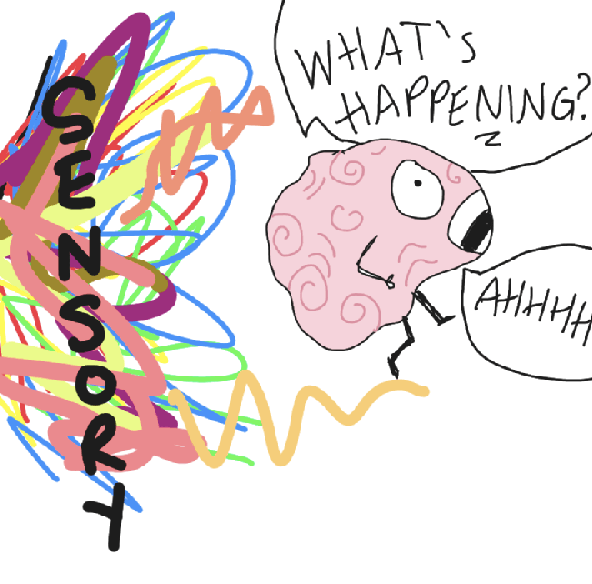
We use our senses for everyday functions such as self-protection, academic skills, self-regulation, Body awareness, balance, Fine motor skills (hand movements), and Gross motor skills (body movements). Sensory processing is how the nervous system receives messages from our five senses and turns them into meaningful responses.
Sensory Processing Disorder (S.P.D.) comes about when the brain inefficiently processes sensory messages coming from a person’s own body and his or her environment.
As much as sensory processing differences/challenges exist, S.P.D. is not considered a disorder by psychiatrists and other mental health professionals. Some doctors consider S.P.D. a symptom of other disorders (A.S.D., Hyperactivity, Attention Deficit Disorder, anxiety, etc.)
Patterns of Dysfunction in Sensory Processing Disorder
When a child has S.P.D., the underlying problem could be one or more patterns of dysfunction. These patterns include Sensory Modulation Dysfunction, Sensory Discrimination Dysfunction, and Postural Disorder.
1. Sensory Modulation Dysfunction
When a child has Sensory Modulation Dysfunction, they will be over-responsive or “sensory defensive,” Under-responsive or a sensory craver.
a) Over Responsive
The child will be over-responsive to certain sensory stimuli. For example, a child will not wear any clothes with a tag on them; they feel as if something poking them (Tactile challenges). They may not want their hair cut since the shaving machine sounds like a saw machine. In a church setting, they might frequently try to shut their ears since the sound feels like they are in a noisy car or a loud club setting) – Auditory challenges.
When in a bright environment, the child will constantly shut their eyes since they feel like a spotlight is on their face (visual challenges). They might fight and scream while approaching an elevator or escalator because when on it, they feel it is like one of the tests at the National Aeronautics and Space Administration (NASA) – Vestibular challenges.
They will avoid certain food textures such as Yogurt with a little bit of fruit, mashed foods, foods with soup, etc (Oral Motor).
This is contributed significantly by oral motor sensitivity and poor oral-Motor Skills. When a child has sensory over responsiveness, they can either be fearful and cautious or hostile and defiant.
b) Under Responsive
The under-responsive child’s attention will not be aroused by the various sensory stimuli as expected. They will not participate in play or other social activities since they do not get sensory feedback.
c) Sensory Craver
For the sensory craver, they seek intensity. They will spin, jump, constantly bite non-food objects, and touch and smell people and objects. Generally, they are constantly on the ‘go.’
2. Sensory Discrimination Dysfunction
When a child has Sensory Discrimination Dysfunction, they will have difficulty differentiating between and among sensory stimuli. They find it hard to gauge how hard I should throw the ball, how loud is his/her voice, and how hot or cold is the surface?
3. Postural Disorder
When a child has a postural disorder, he/she will have difficulty with movement patterns, balance, and using both sides of the body together (bilateral coordination). Activities such as getting up and down steps will be complex; balancing on pavement will be a tall order, and tying shoelaces will be extremely taxing for them.
Sensory Overload and Meltdowns

A meltdown is a way of responding to extreme stress and sensory overload. It is not limited to screaming and shouting but can also include self-injury. Stressors that lead to meltdowns can be internal (e.g., anxiety) or external (e.g., a noisy environment). Sensory processing difficulties can also be stressors; identifying a child’s sensory triggers can help avoid an imminent meltdown.
Sensory Integration Therapy - Treating Sensory Processing Disorders
Sensory Integration Therapy is necessary for treating a child with S.P.D.
This form of Therapy calms or resets a child but does not cure it. Children with Sensory Processing Disorder don’t “grow out of it,” but they find ways to cope through sensory Integration. Sensory Integration prompts self-regulation. It enables the child to know what they need regarding sensory stimuli at any particular time and how to safely access them.
Who does Sensory Integration Therapy?
Sensory Integration Therapy is done by a qualified Pediatric Occupational Therapist (OT) with knowledge and experience in Sensory Integration. The pediatric O.T. does assessments and evaluations, enabling them to know which sensory factors are affected.
Once this is done, they start the sensory integration therapy, which will involve fun activities that will aid the child in learning how to appropriately process the different sensory stimuli. In addition, the Pediatric O.T. creates a Sensory Diet (A program of sensory activities) for the school and home environment.
In some cases, a sensory gym is built at home to enable the child to participate in the sensory circuit effectively and have a multi-sensory environment at home.
Sensory diet Toys, Equipment and tools
Below is a list of some sensory diet Toys, Equipment, tools, and the various sensory areas the items aid in.
- Chewys – Oral Motor.
- Vibrating Toothbrush – Oral Motor.
- Therapressure Brush – Tactile.
- Theraputty/slime – Tactile and or Proprioceptive.
- Ball baths – Proprioceptive and or tactile.
- Weighted Jacket – Proprioceptive.
- Weighted Blanket – Proprioceptive.
- Weighted therapy ball – Proprioceptive.
- Trampolines – Proprioceptive and or Vestibular.
- Swing (Indoor or Outdoor) – Vestibular.
- Noise cancellation Headphones – Auditory.
- Scented toys – Olfactory.
- Glow in the dark toys – Visual.
- Sensory bottles – Visual.
Sensory Integration in a School Environment

Students with S.P.D. have significant inconsistencies and fluctuations in processing information. In a school setup, they may show the following signs:
- Have difficulty regulating their arousal levels: either hyperactive (always on the go) or hypoactive (rarely moves even in the playground).
- Are distractible and/or need help paying attention.
- Chews/licks on non-food objects.
- Avoids getting their hands messy.
- Are sensitive to certain fabrics; avoid wearing clothes made of cloth they can’t tolerate.
- Can’t stay in line when it is time to “line up.”
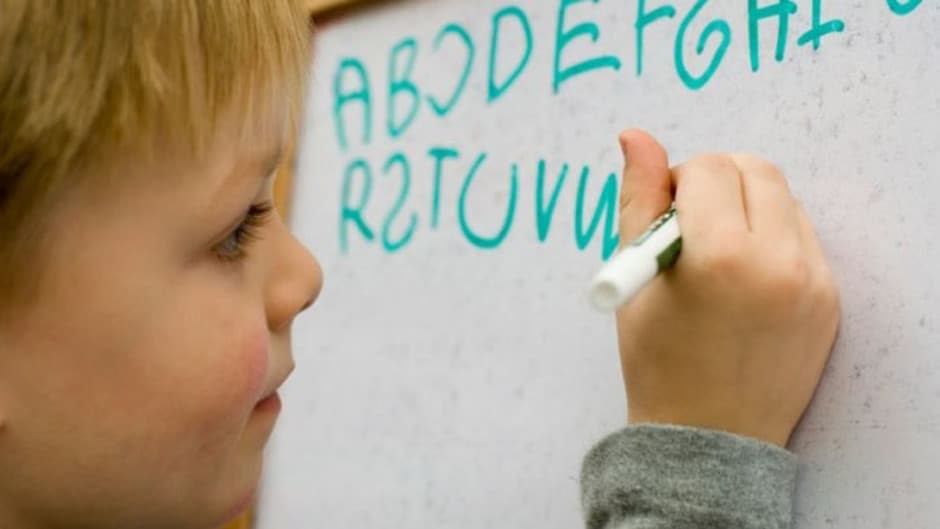
- Have sloppy, disorganized handwriting.
- Demonstrate letter reversals.
- Shouts or whispers constantly while talking.
- Poor use of space on paper/difficulty with spatial concepts. Their writing will be too spaced or too close to each other. They might also need help to stay between page boundaries.
- Need help following directions as to how to perform a task.
- Need better organizational skills, academics, as well as self.
- Difficulty in gross motor skills (e.g., throwing and catching a ball)
- Tires quickly, especially when standing or holding a particular body position.
- Play too roughly or avoids playing.
- Avoids certain textures like sand etc.
- Difficulty going to sleep during nap time.
Teachers, parents, and therapists can work together to adapt to the child’s school environment. These adaptations involve:
Developing a quiet corner or sensory corner
Having a sensory basket in this corner is essential. This will give the child various options for what to do while there. A bean bag chair is also a great asset in this corner. Clear, consistent rules regarding what is acceptable in the corner and what is not should be communicated verbally and visually to the student. A small black tent can work if a quiet corner is hard to create due to limited space.
Decrease Distraction
A separate working table can be created if the student does not like noisy areas. When the student feels the noise levels increasing, they can work at their quiet workstation. If it is during lunch break and the hall is very noisy, let the students wear their noise-cancellation headphones; this enables them to enjoy lunch with their peers. If the student is visually distracted by the lights in the class, turn the lights off and provide a temporary widow blinder.
Sensory Diets
Creating individualized sensory diets would have great alerting, organizing, and calming activities targeted to meet the student’s needs. The sensory diet can also be a whole class activity, e.g., jumping jacks or running one lap in the field. These are great alerting activities that all the students can participate in.
Sensory Playgrounds
The school can have a playground with sensory play equipment such as trampolines, swings, small mountain climbers, tunnels, sit and spins, stand and spins, etc. This playground will encourage the children to perform various sensory circuits.
In Conclusion
Understanding Sensory Processing Disorders is essential as it aids in helping the child with Sensory difficulties. It is also important to determine if a child’s sensory processing difficulties are caused by or related to Autism Spectrum Disorder. A qualified Pediatric O.T. will provide proper Sensory Integration Therapy using suitable sensory diet toys, equipment, and tools.
Do you have any experience with Sensory Processing Disorders? Do you have any questions regarding Sensory Processing Disorder or Autism Spectrum Disorder?
Leave a comment or chat on WhatsApp. You can also get in touch with us.
Don’t forget to share widely.
-
Previous Post
Book Review: The Gift of Dyslexia




Niven
November 12, 2019Nice...very educative
Dynamic Occupational Therapy
November 13, 2019Thank you very much. Let us know if you have any questions.
June kings
November 13, 2019How can I get the services
Dynamic Occupational Therapy
November 13, 2019Hi June, Please get in touch with us via WhatsApp chat or email for more information.
Cgathoni
November 15, 2019good read👌👍
Dynamic Occupational Therapy
August 3, 2020Thank you Cgathoni.