
Back in August, we had the privilege of attending a symposium whose main objective was encouraging Medical practitioners, including Occupational therapists to achieve Excellence in ADHD Management. It was amazing to hear from Prof. Jan Buitalaar, Vice President of the World ADHD Federation, Dr. Josephine Omondi, Dr. Susan Wamithi, and Dr. Judy Kamau.
We are sharing a few take-homes from this special symposium.
Take Home #1: ADHD is on an Increase in Kenya
A study done by several clinicians in Kenya showed that cases of ADHD have increased from 18% to 45%. The study involved doing various tests, including the Vanderbilt Assessment Scale, on children taken to the hospital by their parents. From the study, the main reasons highlighted that brought the children and/or adolescents to the hospital were:
- School Demands and failures
- Aggression and violent behavior
- Gustatory problems – constipation
- High-risk behaviors in Pre-adolescents and Adolescents.
The main symptoms of ADHD observed were:
- Hyperactivity: The student may found hard to sit still for the same period as their peers and would constantly fidget.
- Inattention: The student’s attention span was brief compared to his/her peers. They were easily distracted, and once distracted, they found it hard to get back on course.
- Impulsivity: The student would constantly be on ‘the go,’ have trouble waiting his turn, and frequently interrupt a conversation. This was still gauged by his/her peers.
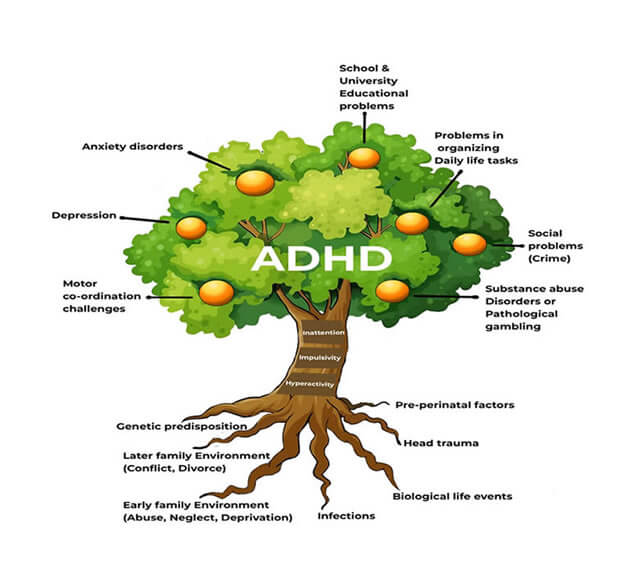
The ADHD Tree
To help us get a better understanding of ADHD, we got to create the ADHD Tree. The ADHD tree gives an artistic representation of ADHD, showing probable causes, core symptoms, and the presentation of the core symptoms.
- The roots represent the probable causes of ADHD.
- The tree trunk represents the three core symptoms of ADHD.
- The fruits represent the various presentations of the core symptoms.
The Connection Between Crime and ADHD in Kenya
Research conducted in one of the Prisons in Kenya found that some inmates had ADHD. Does this mean there is a direct connection between crime and ADHD in Kenya?
The research results indicated that; When aggression and Violence are combined with high-risk behaviors, chances are high that the person will get on the wrong side of the law. In addition, if a pre-adolescent/Adolescent is rejected and neglected due to their ADHD symptoms, they are susceptible to crime.
The impulsive nature of ADHD adolescents also predisposes them to crime since they will find it difficult to or will not try to figure out the consequence of their actions from a long-term perspective.
Take Home #2: ADHD Interventions in Kenya
The various interventions are but are not limited to Medication, Mindfulness Training, Gaming, Counselling, Occupational Therapy, Cognitive Behavior therapy, Elimination Diet, and Sports/aerobic activities.
Whichever form of treatment the patient and or the caregiver chooses, the intervention needs to be:
- Patient-focused: The treatment would focus on reducing the symptoms of ADHD (impulsivity, hyperactivity, and Inattention). Different approaches can be used depending on the patient and his/her family. Some prefer to combine the various options.
- Parent-focused: Parents require frequent training to understand what ADHD is and the various ways they can support their children. The training will aid the parents in understanding the impact of ADHD on the rest of the family, the impact on their marriage, and finally, the impact on their mental health. The parents require support groups to help them cope.
- School-focused: Teachers need knowledge of ADHD; this will aid them in knowing the nature of this disorder. During the training, they will learn behavior modification techniques to be able to increase desirable behaviors and decrease bad behaviors.
The main point is that if you impose a mode of treatment that is not accepted, it will fail. The patient, family, and school need to be on the same page, and the collaboration of the three will improve the quality of life of the client with ADHD.
During treatment, it is essential to identify the positive attributes of the patient with ADHD. Many people with ADHD have the privilege of being more creative. This is further expounded in this article by the Scientific American
Take Home #3: Tips to Manage ADHD in Kenya
Tips for Clinicians/OCcupational Therapists
The clinician has an integral role in assessing and later diagnosing ADHD. They have the privilege of interacting with the client (child with ADHD) and his/her family during the assessment and intervention period. Here below are a few tips for the clinician.
- After the assessment and diagnosis, ask the client, parent, and/or other caregivers about their view on the problem and its solution, and then jointly develop a treatment plan.
- Introduce informative self-help materials.
- Keep yourself updated on the various services the student is receiving and how each is progressing.
Tips for Parents and Caregivers
Parents spend a lot of time with their children, and often they are the first ones to identify their children’s challenges. Once a diagnosis is made, it is essential to:
- Strengthen a positive relationship with your child. Take time to participate in their interests.
- Strive to catch your child doing right and praise them often.
- Take care of yourself (your emotional well-being); giving what you don’t have is very hard.
- Establishing clear rules and following through constantly and consistently with positive and negative consequences is essential.
Tips for Teachers and School Administrators
Apart from the parents, the teachers spend a lot of time with the clients and are crucial in guiding the parents and the clinicians on the effectiveness of the intervention plan. But to be able to do this, the teacher needs to:
- Be knowledgeable about ADHD and the various treatments the student is receiving.
- Keep in touch with the therapist, learn as much as possible, and give feedback about the student. As a teacher, you can notice changes in the student, e.g., when they start medication; how is their attention and concentration throughout the day? Is there a change in the student’s behavior? A teacher can keep a detailed behavior chart that can guide any therapist.
- Build a positive relationship with the student.
- Establish clear rules consistently.
- Follow through with the positive/negative consequences.
Conclusion
As stated in take home #1, ADHD is increasing in Kenya. To help children, preadolescence, adolescents, and adults with ADHD, it will take a team effort between parents, teachers, and clinicians. The big question is, how can we achieve this in Kenya? Can we make it happen?
I would love to hear your views, suggestions, and comments on how we can come together to effectively manage ADHD in Kenya.
Leave a comment below or let’s chat on WhatsApp. You can also get in touch with me if you have any questions regarding ADHD.
-
Previous Post
How to Safely Feed a Child With Cerebral Palsy



