Feeding involves many processes. Naturally, we know of the two basic steps: chewing and swallowing. However, chewing and swallowing are more complex than we assume. They are relatively complex and involve almost 50 pairs of muscles and nerves. There are three phases involved in chewing and swallowing:
- Oral preparatory and transport phase: The mouth muscles perform a voluntary step. It includes opening and closing the mouth, mastication(chewing), and mixing the food with saliva.
- The pharyngeal phase starts when the bolus (formed in the first phase) enters the throat. The beginning of this phase is voluntarily followed by an involuntary action of the bolus entering the esophagus.
- Esophageal phase: The bolus moves further down the esophagus to the stomach.
For the child with Cerebral Palsy, the first phase is usually challenging.
Feeding difficulties for a child with Cerebral Palsy
Children with cerebral Palsy frequently have feeding challenges from as early as breastfeeding. This is due to varying neuromuscular difficulties. Parents/caregivers need to know possible interventions to prevent choking when feeding a child with Cerebral Palsy.
This article will look at four main areas that will enable you to safely feed a child with Cerebral Palsy. These include Feeding position, Feeding Utensils, Change in food and liquid consistency, and encouraging chewing.
1. Proper Feeding Position
When feeding a child with Cerebral Palsy, it is essential to consider their feeding position. From breastfeeding an infant to feeding solids to a growing child, a proper feeding position will help to prevent the child from choking.
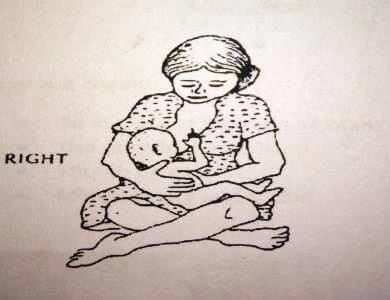
Feeding Position For a Breastfed and or Bottle Fed Baby
While breastfeeding a baby with Cerebral Palsy, position him/her in a half-sitting position with his/her head slightly forward. To keep the head from pushing back, hold the shoulders forward, keep the hips bent, and push firmly on the chest.

While bottle-feeding the baby, position the baby so that the head is slightly forward and the bottle comes from in front, not above.
Feeding Position for an Older Child with Cerebral Palsy
The child must be upright either on a feeding chair or an adapted wheelchair that has a feeding table. The Rifton Hi-Lo Activity Chair (image below) helps to stabilize the feet, hips, chest, and head areas. Once stabilized, the child can focus on feeding. In addition, the chair also encourages symmetry and eye contact during feeding.

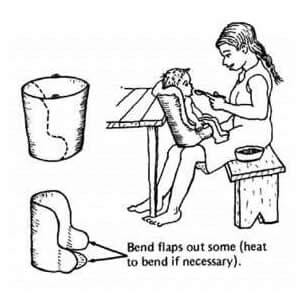
Various adaptations can be made even without a feeding chair, as seen in the next photo. The most important is that the child is upright and the points of control are stabilized.
2. Use Adapted Feeding Utensils
A child with Cerebral Palsy requires adapted feeding equipment to feed efficiently and promote self-feeding. Self-feeding is an essential skill that should be encouraged. Let the child touch and see food; this enables the child to get used to how the food feels. Make it a habit to eat with the child to see how to feed them, then let them experiment.
For example, using an adapted or cut-out cup will enable the child to drink and not have to tilt their head back.


3. Change the Food and Liquid Consistency
When feeding a child with Cerebral Palsy, it is recommended to change the consistency of foods (textures, temperature, fluidity, and tastes). The benefits of changing food consistency include the following:
- Ensures that swallowing is safe and that the food/liquid does not enter the airway in case of delayed swallowing.
- Enhances sensory stimulation; different textures and food temperatures may stimulate oral movement and trigger swallowing.
Gradually increase the density/thickness of the food and later on the ‘lumpiness’ of the food. However, ensure the feeding is safe and that the child is not choking or coughing.
4. Encourage chewing
While feeding, place the food on the side of the child’s mouth, between the teeth, to encourage chewing and side-to-side tongue movement. Initially, use softer foods, such as bananas, well-cooked vegetables or fruits, macaroni, and bread. Place foods on the weaker side.
Some children might have great difficulties feeding and chewing even with the above recommendations; if this happens, consult a specialized medical practitioner, speech and language therapist, and an occupational therapist to further assist.
-
Previous Post
School Based Project at Nakeel Special Unit